FATIGUE, PAIN, DEPRESSION, COGNITIVE CHANGES: INVISIBLE SYMPTOMS OF MS
By: Matthew Sacco, PhD, Tracy Walker, FNP-C, WOCN
Fatigue, Pain, Depression, Cognitive Changes: Invisible Symptoms of MS
Matthew Sacco, PhD and Tracy Walker, FNP-C, WOCN
Can MS be invisible?
With symptoms like fatigue, depression, and cognitive dysfunction, many people with MS are fighting battles that others can’t see. How do you manage these symptoms? Why do they occur? And what do you do when other people are saying to you, “But you look so good!”?
What Does MS Feel Like?
When you disclose your MS diagnosis, many people (often with kind intentions) don’t believe what they cannot see, replying with “You don’t look like you have anything wrong with you.”
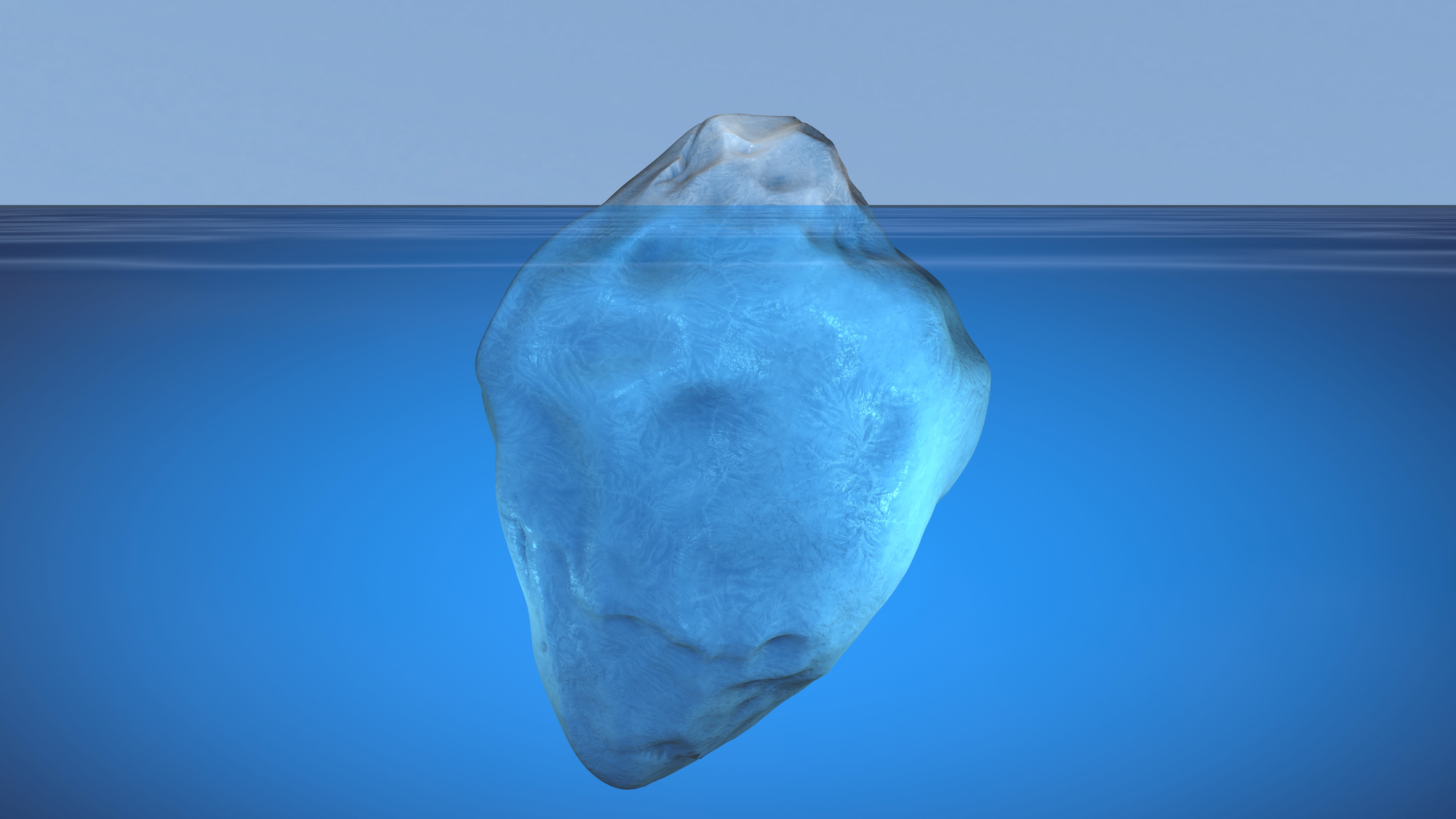
The next challenge you face is explaining that looks can be deceiving. There is an ongoing war just under the surface and out of plain sight that is being waged on your body by MS. The battles are unpredictable, can change day to day, and they feel different for everybody.
What are Some of the Most Common Invisible Symptoms of MS?
Fatigue
Fatigue is often described as a lack of energy that occurs on a regular/daily basis. It is not the same thing as being tired. Becoming tired is something that happens to most people from time to time and is completely relieved by getting a good night’s sleep. Fatigue is excessive and entire body tiredness that is not relieved by getting a good night sleep. Up to 80% of people with MS experience MS fatigue!
Depression or Depressive Symptoms
At least 50 percent of individuals with MS report significant symptoms associated with depression. These symptoms can include feeling down, blue, and sad for extended periods of time. Symptoms can also include a lack of energy or motivation, irritability, frustration and experiencing a “shorter fuse.” While having these symptoms does not necessarily mean a person is experiencing clinical depression, it is important to note the changes in mood as they occur and seek help when the symptoms start to interfere with functioning.
Cognitive Dysfunction
Changes in cognitive functioning are often associated with MS. In fact, it has been estimated that 40-65% of PwMS experience some degree of change over the course of the disease. Symptoms often can include: slowed processing speed, memory impairment, impaired attention/concentration, impaired executive functions, impaired spatial relations and impaired word-finding ability.
Spasticity
Spasticity is a common symptom in MS and frequently occurs with lesions in the spinal cord. Spasticity refers to involuntary muscle firing and generalized increase in muscle tone that can occur within any muscle group, but is most common in the legs. It can range in severity from mild to severe and can result in pain and mobility issues.
Pain
The experience of pain was not something that was previously recognized as a significant symptom of MS. Now however, most professionals do in fact recognize pain as a relatively common symptom associated with MS. It can occur for a number of reasons.
Is Your MS Pain Acute or Chronic?
Pain in MS can be acute or chronic. Acute pain occurs suddenly such as during a relapse or in the setting of fever, infection, or other precipitating factors. Chronic pain with MS can feel like acute pain and present that way to a doctor, and it can worsen when relapse or other factors such as infection occur. However, unlike acute pain, chronic pain does not resolve completely when those issues are treated. Chronic pain is often caused by multiple factors, so you may need a multidisciplinary approach to treat it (meaning, your neurologist and other specialists should collaborate on a treatment plan).
What Types of Pain Are Common with MS?
- Trigeminal neuralgia– stabbing pain in the face and jaw worsened by cold temperatures and often mistaken for dental issues.
- Lhermitte’s sign – shock like sensation that often runs from head down to spine and into the arms and legs when bending the neck.
- MS Hug – squeezing like sensation around the torso.
- Paroxysmal spasms – intermittent spasms of muscles (EG: arms and legs) that can occur at any time.
- Neuropathic pain – often presents as burning stinging pain, painful numbness, or other uncomfortable sensations to specific areas such as hands and feet or more generalized throughout the body.
- Musculoskeletal pain – pain caused by strain on muscles and joints that are needed to compensate for weakness or spasticity in other muscles in order to maintain function. A common example is back pain from altered gait.
How Do You Manage Fatigue, Pain, and Other Invisible Symptoms?
Treating and managing the invisible symptoms of MS is often most effective when utilizing a holistic and multifaceted approach. First, ensure that you have communicated with your healthcare team, including your neurologist, primary care provider, and anyone else helping you manage your health. Tell them what you are feeling, and if they don’t recommend it themselves, ask for a thorough examination of your physical health.
Health Check-Up
Since MS symptoms can be worsened by comorbidities (that is, other health issues that are not caused by your MS), it’s important to identify and treat those health issues as a first step. For example, someone with MS and diabetes will first need to make sure their blood sugar levels are in check. Or someone with thyroid or cardiovascular issues will need to be identify and address these issues, which may be triggering a spiral of MS symptoms.
In addition to getting a check-up, know that probably the most important behaviors that affect your MS symptoms are the ones that are in your control.
Healthy Diet
Remember, there is no “MS diet”! Everyone’s diet goals will be different and should be made in consultation with your healthcare team. But most of us (living with MS or not) would benefit from eating a diet that consists of a lot of green leafy vegetables, lean meats, and fish (or other foods rich in omega-3 fatty acids).
Exercise
Talk with your neurologist and PT to help establish an exercise routine that will work for you. As little as 20 minutes of moderate exercise per day can pay huge dividends for your health!
Remember, all movement counts – you don’t need to tackle a workout all at once.
You can build up your endurance and strength by fitting in exercise snacks while you go through your day. You can also prioritize the activities that are most fun for you. Walking with friends, getting in the pool, or practicing yoga are all great for your health!
Activity Pacing
Avoid the pitfall of cramming everything in on the days when you feel especially energized. This is typically followed by a period of underactivity and recovery. Pace yourself!
Sleep
Establish a regular and consistent sleep schedule. This can be difficult with MS, however but aim to start with a sleep routine that is as consistent as possible.
Relationships
Aim for a healthy variety of relationships in your life. This includes family relationships as well as friends, other acquaintances, and even support groups. (Hint: Can Do MS Programs can be a great place to connect).
Communication
Have open and honest dialogue about your symptoms (as necessary). Educate your loved ones and friends about MS invisible symptoms.
And if you are tired of carrying that burden alone, here’s a tip: Can Do MS Programs are always open to anyone in your support network. These can provide a great deal of education for spouses, family, or friends!
Help/Assistance
Reach out to professionals for help. Mental health providers, rehabilitation specialists, and nurses can all help to ensure you are doing everything in your power to manage symptoms.
Talking About Invisible Symptoms
Since others cannot read your mind or feel what you feel, here are a few ways to explain invisible symptoms.
- The effects of invisible symptoms can hit in waves. There will be times that no matter what you do, you just cannot shake it.
- Yes, there are strategies to manage these symptoms. But these tools offer what is likely the best chance to manage the symptoms of MS over the long haul. Your loved ones can’t expect you to get better overnight.
- Invisible symptoms that are not managed well often fuel one another in a vicious cycle. Mood problems often make the experience of pain worse, which compromises cognitive functioning, then worsens spasticity. Patterns like this can play out over and over with each cluster of symptoms.
For you to mitigate the impact of invisible symptoms (and the heartache of having loved ones who don’t understand), keep the lines of communication open. It may take patience, but it’s important for you to talk to your friends, family, and especially your healthcare team about the invisible symptoms you face with MS.
SOURCE: Can Do MS