
What is MS?
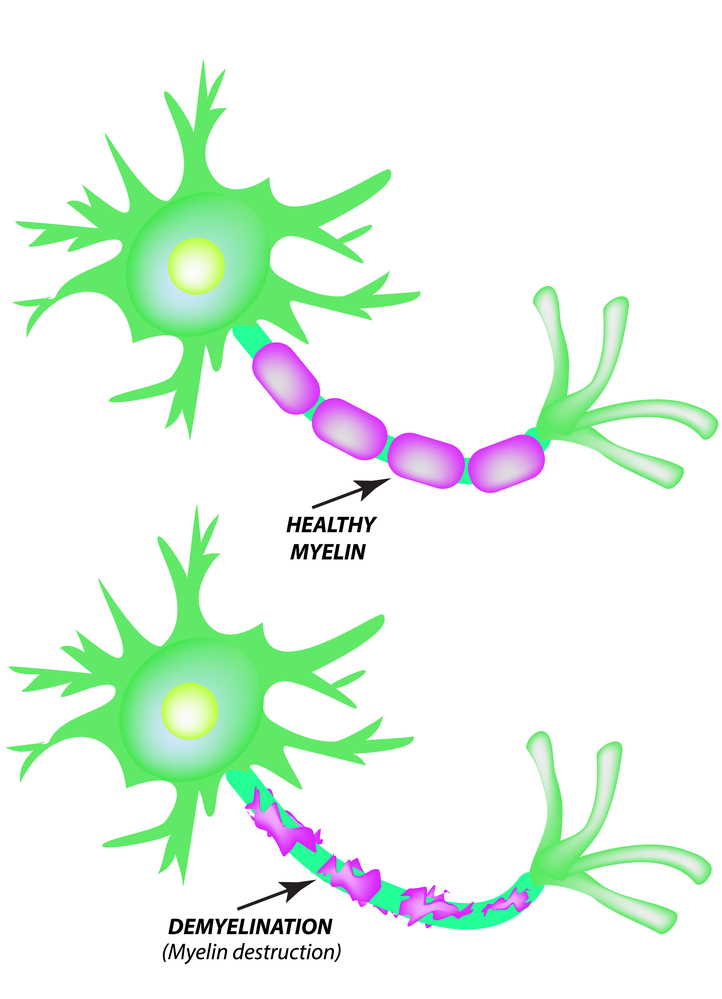
Multiple Sclerosis (MS) is currently classified as an autoimmune disease of the Central Nervous System (brain, spinal cord). This disease attacks the Myelin which is the protective covering of the nerves, causing inflammation and often damaging the Myelin. The Myelin is necessary for the transmission of nerve impulses through nerve fibres.
If the damage to the Myelin is slight, nerve impulses will travel with minor interruption; however, if the damage is substantial and if scar tissues replace the Myelin, nerve impulses maybe completely disrupted and the nerve fibres can be damaged.
Multiple Sclerosis is unpredictable and can cause symptoms such as extreme fatigue, lack of coordination, weakness, tingling, impaired sensations, vision problems, bladder issues, cognitive impairment and mood changes.
The effects of MS can be physical, emotional, and financial. Currently, there is NO CURE. Each day researchers are learning more about what causes MS and are finding ways to prevent it or at least slow down the progression of MS!
Types of MS
Clinically Isolated Syndrome (CIS)
CIS is a first episode of neurologic symptoms caused by inflammation and demyelination in the central nervous system. The episode, which by definition must last for at least 24 hours, is characteristic of multiple sclerosis but does not yet meet the criteria for a diagnosis of MS because people who experience a CIS may or may not go on to develop MS.
When CIS is accompanied by lesions on a brain MRI (magnetic resonance imaging) that are similar to those seen in MS, the person has a high likelihood of a second episode of neurologic symptoms and diagnosis of relapsing-remitting MS. When CIS is not accompanied by MS-like lesions on a brain MRI, the person has a much lower likelihood of developing MS.
The 2017 diagnostic criteria for MS make it possible to diagnose MS in a person with CIS who also has specific findings on brain MRI that provide evidence of an earlier episode of damage in a different location and indicate active inflammation in a region other than the one causing the current symptoms.
Like MS, CIS is not directly inherited, and it is not contagious. CIS is two to three times more common in women than men. Seventy percent of people diagnosed with CIS are between the ages of 20 and 40 years (average 30 years) but people can develop CIS at older or younger ages.
According to the 2017 revisions to the diagnostic criteria, when CIS is accompanied by evidence on MRI that another episode has occurred, the diagnosis of MS can be made. The presence of oligoclonal bands in a person’s cerebrospinal fluid can also help make the diagnosis.
A person with CIS, by definition, is experiencing the first episode of symptoms caused by inflammation and demyelination in the CNS; a person with MS has experienced more than one episode.
With CIS, an MRI may demonstrate damage only in the area responsible for the current symptoms; with MS, there may be multiple lesions on MRI in different areas of the brain.
As MRI technology improves, the diagnosis of MS will be made more quickly and easily. In the meantime, individuals with CIS who are considered at high risk for developing MS may now be treated with a disease-modifying therapy that has been approved by the U.S. Food and Drug Administration (FDA) for that purpose. Early treatment of CIS has been shown to delay onset of MS.
Secondary progressive MS (SPMS)
SPMS follows an initial relapsing-remitting course. Some people who are diagnosed with RRMS will eventually transition to a secondary progressive course in which there is a progressive worsening of neurologic function (accumulation of disability) over time. SPMS can be further characterized as either active (with relapses and/or evidence of new MRI activity during a specified period of time) or not active, as well as with progression (evidence of disability accumulation over time, with or without relapses or new MRI activity) or without progression.
 Disease activity can occur in SPMS over time; however each person’s experience with SPMS will be unique. SPMS follows after relapsing-remitting MS. Disability gradually increases over time, with or without evidence of disease activity (relapses or changes on MRI). In SPMS, occasional relapses may occur, as well as periods of stability.
Disease activity can occur in SPMS over time; however each person’s experience with SPMS will be unique. SPMS follows after relapsing-remitting MS. Disability gradually increases over time, with or without evidence of disease activity (relapses or changes on MRI). In SPMS, occasional relapses may occur, as well as periods of stability.
Relapsing-remitting MS (RRMS)
RRMS – the most common disease course – is characterized by clearly defined attacks of new or increasing neurologic symptoms. These attacks – also called relapses or exacerbations – are followed by periods of partial or complete recovery (remissions). During remissions, all symptoms may disappear, or some symptoms may continue and become permanent. However, there is no apparent progression of the disease during the periods of remission. RRMS can be further characterized as either active (with relapses and/or evidence of new MRI activity over a specified period of time) or not active, as well as worsening (a confirmed increase in disability following a relapse) or not worsening.
Approximately 85 percent of people with MS are initially diagnosed with RRMS.
Disease activity can occur in RRMS over time; however each person’s experience with RRMS will be unique. Following a relapse, the new symptoms may disappear without causing any increase in level of disability, or the new symptoms may partially disappear, resulting in an increase in disability. New lesions on MRI, as shown by the arrows, often occur as part of a relapse. However, new MRI lesions indicating MS activity may also occur without symptoms of which the person is aware.
Primary progressive MS (PPMS)
PPMS is characterized by worsening neurologic function (accumulation of disability) from the onset of symptoms, without early relapses or remissions. PPMS can be further characterized as either active (with an occasional relapse and/or evidence of new MRI activity over a specifperiod of time) or not active, as well as with progression (evidence of disability accumulation over time, with or without relapse or new MRI activity) or without progression.
Approximately 15 percent of people with MS are diagnosed with PPMS.
 Disease activity can occur in PPMS over time; however each person’s experience with PPMS will be unique. PPMS can have brief periods when the disease is stable, with or without a relapse or new MRI activity, as well as periods when increasing disability occurs with or without new relapses or lesions on MRI.
Disease activity can occur in PPMS over time; however each person’s experience with PPMS will be unique. PPMS can have brief periods when the disease is stable, with or without a relapse or new MRI activity, as well as periods when increasing disability occurs with or without new relapses or lesions on MRI.
Source: National MS Society
Very often people with MS hear “you don’t have to do anything but sit there”.
What is MS? A presentation by MY MS FAMILY
Join our eMailing List
Have you recently been diagnosed with multiple sclerosis or do you care about someone who has?
If you provide your name and email address, we'll send you regular updates about our activities as well as important topics related to life with MS.
Please NOTE: Completing this form gets you on our mailing list but not paid membership status.
If you would like to tap into our membership benefits, please use this link.
We will never share, rent, or sell your personal information. Never gonna happen. You have our word on that.
